Many aspects of our lives change with age. Our energy levels, metabolism, and how we sleep. While it’s common for older adults to report difficulty falling asleep or staying asleep throughout the night, this isn’t just a natural part of aging. There are deeper biological, psychological, and environmental factors at play.
Let’s explore why older adults struggle with sleep and what can be done about it.
The Biological Clock Shifts in Older Adults
Circadian Rhythm Changes: The circadian rhythm controls our sleep-wake cycle. This rhythm is governed by the suprachiasmatic nucleus (SCN) in the brain. The SCN becomes less sensitive to light cues in older adults. This desensitization means that older adults do not respond as strongly to natural light during the day or darkness at night. This leads to a misalignment of their sleep schedule.
Many older adults experience Advanced Sleep Phase Syndrome (ASPS). In this phenomenon, they feel sleepy earlier in the evening and wake up much earlier than desired (often between 3-5 a.m.). This shift can be frustrating, especially if social or family obligations require staying up later.
Melatonin regulates sleep onset. With age, melatonin production decreases. The reduced melatonin makes it harder for older adults to fall asleep and stay asleep.
Light Exposure and Its Role: Light exposure plays a crucial role in maintaining a healthy circadian rhythm. Older adults spend more time indoors. This reduces their exposure to natural light. This lack of light exposure further disrupts the circadian rhythm.
Exposure to bright light can help reset the circadian rhythm and improve both sleep onset and duration. Morning sunlight exposure, in particular, has been shown to be effective in delaying the early onset of sleepiness.
Changes in Sleep Architecture
Sleep Stages: Sleep is divided into several stages, including non-REM (NREM) sleep and REM sleep. NREM sleep consists of three stages: light sleep (Stage 1), slightly deeper sleep (Stage 2), and deep sleep (Stage 3). Deep sleep is essential for physical recovery, immune function, and memory consolidation.
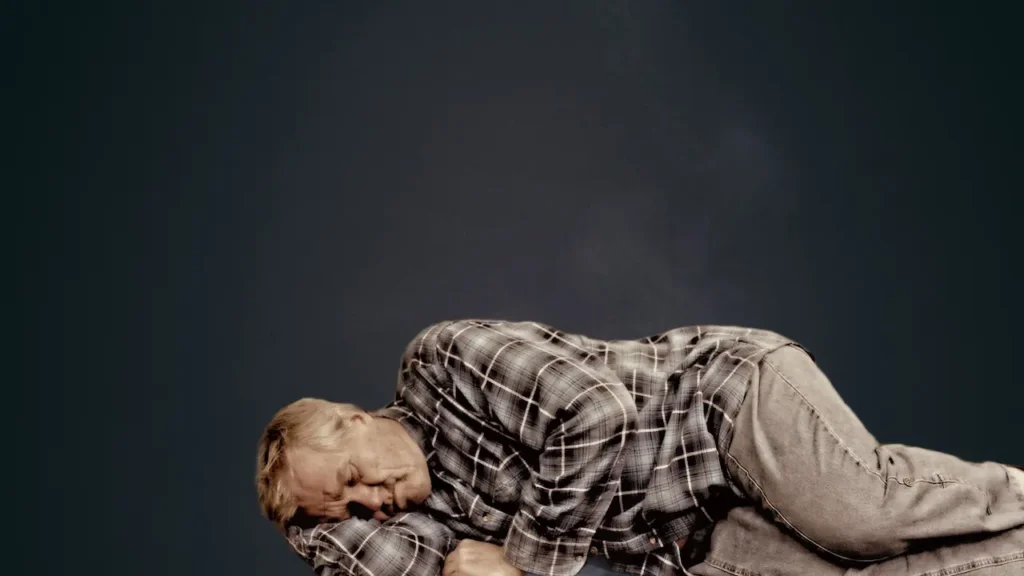
As we age, the amount of time spent in deep sleep decreases significantly. By the age of 60, many people spend only about 20% of their total sleep time in deep sleep, compared to around 40% in younger adults. This reduction in deep sleep makes older adults susceptible to waking up frequently during the night and feeling less refreshed in the morning.
Older adults tend to spend more time in lighter stages of sleep. Light stages of sleep are easier to disrupt. Any minor disturbances cause them to wake up. This increased sensitivity to external stimuli contributes to fragmented sleep patterns.
REM Sleep Alterations: REM sleep, the stage associated with vivid dreaming and emotional processing, also changes with age. The intensity and quality of REM sleep declines.
Health Conditions Interfere with Sleep
Chronic Pain: Arthritis, fibromyalgia, and back pain make it difficult to find a comfortable sleeping position. Frequent discomfort leads to frequent awakenings throughout the night.
Respiratory Issues and Sleep Apnea: Respiratory problems worsens at night. Older adults face difficulty breathing. Moreover, sleep apnea—a condition characterized by repeated pauses in breathing during sleep—becomes prevalent with age.
Nocturia: The need to urinate multiple times during the night is another common issue among older adults. This can be caused by various factors, including an overactive bladder, prostate enlargement in men, or medications that increase urine production.
Limiting fluid intake in the evening, avoiding diuretic medications before bed, and addressing underlying medical conditions help reduce nocturia and improve sleep continuity.
Mental Health: Depression and anxiety are closely linked to sleep disturbances. Older adults experience these conditions due to retirement, bereavement, and declining health. Depression, in particular, can lead to early morning awakenings and difficulty returning to sleep. Anxiety often causes racing thoughts that prevent sleep onset.

Cognitive Behavioral Therapy for Insomnia (CBT-I) is a structured program that addresses the thoughts and behaviors contributing to insomnia. It has been shown to be highly effective in treating both primary insomnia and insomnia related to depression or anxiety.
Social isolation and loneliness are significant risk factors for poor sleep in older adults. Feeling disconnected from others can lead to increased stress. Emotional distress negatively impacts sleep quality.
Environmental Factors
Noise Sensitivity: Older adults become sensitive to ambient noises that they previously ignored. Sounds like traffic, neighbors, or household appliances can easily disturb their sleep.
Using earplugs, white noise machines, or sound-absorbing materials in the bedroom can help block out unwanted noise.
Light Pollution: Exposure to artificial light at night can suppress melatonin production and delay sleep onset.
Blackout curtains, eye masks, and dimmer switches can minimize light exposure in the bedroom. Avoiding screens (TVs, smartphones, tablets) at least an hour before bed is also recommended to allow the brain to wind down naturally.
Temperature Regulation: Older adults have difficulty regulating their body temperature. This can lead to discomfort during sleep. They may feel too hot or too cold, depending on the season and their individual physiology.
The ideal bedroom temperature for sleep is typically between 60-67°F (15-19°C). Using breathable bedding, adjusting the thermostat, and employing fans/heaters as needed can help maintain a comfortable sleep environment.
Lifestyle Habits Influence Sleep
Napping Patterns: While short naps (20-30 minutes) can boost alertness and performance, excessive daytime napping interfere with nighttime sleep. Older adults who nap for extended periods or late in the afternoon may find it harder to fall asleep at night.
Dietary Choices: Certain foods and beverages either promote or hinder sleep. For example, heavy meals close to bedtime can cause indigestion, while spicy or acidic foods may trigger heartburn.
On the other hand, foods rich in tryptophan (e.g., turkey, nuts, seeds) and magnesium (e.g., leafy greens, bananas) can aid in relaxation and sleep.
Physical Activity: Regular light exercise has numerous benefits for sleep. However, timing is important. Exercise too close to bedtime can elevate heart rate and adrenaline levels. High levels of adrenaline make it harder to fall asleep.
Sleep difficulties in older adults are multifaceted. While aging does present unique challenges to sleep, it’s important to remember that these issues are manageable with the right strategies and support.
By addressing underlying medical conditions, and adopting healthy sleep hygiene practices, older adults can significantly improve their sleep quality. Quality sleep is not just a luxury—it’s a cornerstone of health.
With proactive steps and a holistic approach, older adults can enjoy restful nights and energized days.